Dr. Motiwala
Jan 14, 2025
While brushing and flossing remain crucial for dental health, emerging research reveals that genetics account for up to 60% of cavity risk. Your DNA influences every aspect of oral health, from enamel strength to saliva composition, creating biological advantages or vulnerabilities before your first tooth even emerges. Twin studies demonstrate this clearly – identical twins raised apart show remarkably similar cavity patterns despite different diets and hygiene habits, proving that tooth decay isn’t just about lifestyle choices.
The AMELX, ENAM, and MMP20 genes control enamel formation, creating variations in tooth armor thickness and quality. Some people inherit enamel that’s naturally more porous or thinner, making their teeth inherently more vulnerable to acid attacks. These genetic differences explain why two people following identical oral care routines can have dramatically different cavity experiences. Even the microscopic structure of enamel varies genetically, with some people having tighter crystal formations that better resist bacterial acids.
Your saliva’s cavity-fighting abilities are largely predetermined by genes like CA6 and AQP5 that control its composition and flow. Fast buffers with high calcium content can neutralize acid attacks within minutes, while others may take hours. The FUT2 gene determines whether you’re a “secretor” producing cavity-protective glycoproteins in saliva. These genetic factors create oral environments where bacteria either thrive or struggle, regardless of how often you brush.
Your TAS2R38 taste receptor gene variant doesn’t just make Brussels sprouts taste bitter – it also influences your sugar cravings. “Supertasters” with sensitive bitter receptors often find sweets overwhelming, naturally limiting sugar intake. Meanwhile, those with less sensitive sweet receptors (determined by TAS1R genes) may unconsciously consume more sugar to achieve satisfaction. This genetic lottery significantly impacts cavity risk before willpower even enters the equation.
Your HLA and DEFB1 genes control how aggressively your immune system attacks cavity-causing bacteria. Some variants create an oral environment hostile to Streptococcus mutans, while others allow problematic bacteria to flourish. These genetic differences explain why some people develop cavities despite rigorous hygiene, while others neglect their teeth yet remain cavity-free. Your immune genes also influence gum health, with certain variants increasing periodontitis risk regardless of care.
Modern genetic testing can now identify your inherited risks, allowing personalized prevention strategies. If you have weak enamel genes, high-fluoride toothpaste may be essential. Those with poor saliva genetics might benefit from xylitol products. The new field of “precision dentistry” uses these genetic insights to customize care, moving beyond one-size-fits-all recommendations to strategies that address your biological vulnerabilities.
While you can’t change your DNA, understanding your genetic risks empowers smarter prevention. Those with cavity-prone genetics may need more frequent cleanings, specialized products, or dietary modifications. The key is recognizing that “perfect” oral hygiene looks different for everyone based on their biological inheritance. Your genes set the rules, but your daily choices determine how the game plays out. With the right knowledge and strategies, even those with high genetic risks can maintain healthy, cavity-free smiles for life.
Please click on the NEWS site’s logo below to visit the article.
 |
 |
 |
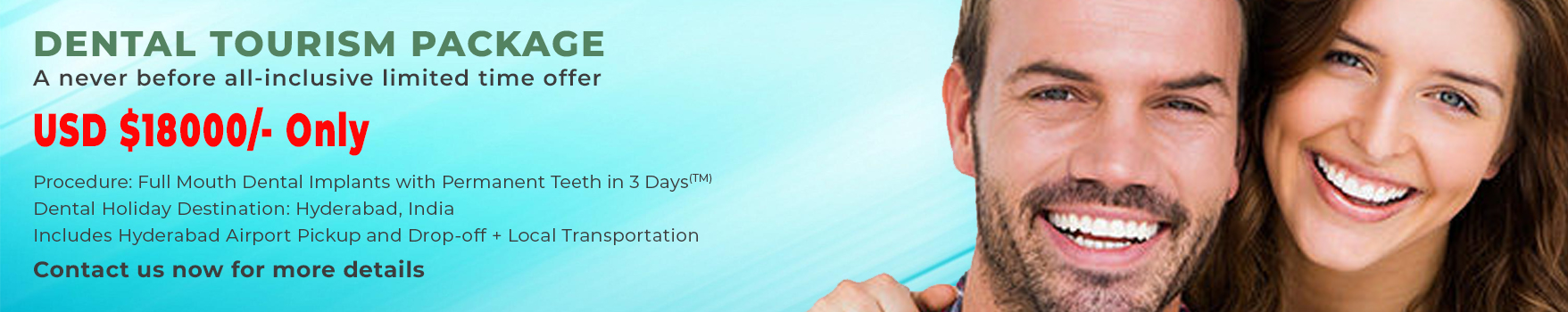
For more details about dental implant prices and your available treatment options, contact Dr. Motiwala’s Dental Clinic & Implant Center at +91 99596 14584. The form on our website’s CONTACT US page also allows you to send us an email. We would be happy to assist you if there is any way we can.